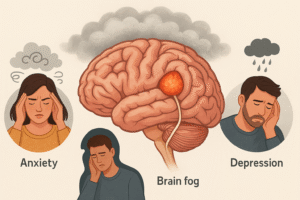
What Is Brain Fog—And How Do Anxiety and Depression Fit In?
“Brain fog” is a term many people use to describe a frustrating mix of cognitive symptoms—sluggish thinking, memory lapses, difficulty concentrating, and mental fatigue. It’s not a formal medical diagnosis, but it’s a very real experience that can disrupt daily life. Many people with acoustic neuroma (AN) report these symptoms, often long before or even after treatment.
Similarly, anxiety and depression are common and often co-exist with brain fog. Anxiety refers to persistent feelings of worry, nervousness, or fear that are difficult to control. It can also cause physical symptoms like rapid heartbeat, muscle tension, and dizziness. Depression, on the other hand, often involves persistent sadness, low motivation, feelings of worthlessness, and changes in sleep or appetite.
While these conditions can overlap in how they make us feel—foggy, tired, or mentally drained—it’s important to understand that brain fog is not simply a by-product of emotional stress. Especially in the context of acoustic neuroma, brain fog has clear physiological origins in the brain itself. Recent research—and the lived experience of many patients—has shown that cognitive symptoms are not just emotional responses, but neurological consequences of the tumour’s effects on the brain.
When the Fog Comes First
For many people, being told they have a brain tumour can understandably trigger anxiety, fear, and even depression. It’s true that being told you have a brain tumour—along with the whirlwind of decisions about surgery, radiation, or just watching and waiting—can lead to anxiety or depression. The fear of the unknown, concern about long-term outcomes, and the sheer weight of the word “tumour” can understandably take a toll on mental health. But in my case, something different happened.
The fog set in long before the diagnosis. Before I knew there was something physically wrong, my mind began to behave differently. My thoughts slowed. My ability to focus scattered. And most unsettling of all, I began to avoid things I used to do confidently—like driving.
That avoidance wasn’t rooted in fear of an accident—it was something much deeper. I felt disconnected from space, like I couldn’t process where I was in relation to other objects. I couldn’t “read the road” the same way. My vision became narrowed, my attention overly fixed on small visual details, while I lost grasp of the wider spatial context around me. This strange phenomenon, I now know, has a fancy name: visuospatial dysfunction.
Yes, like anyone, I’ve had emotional ups and downs in life—times where stress or sadness clouded my thinking. But this fog felt different. Heavier. More mechanical. It wasn’t just mood-related—it felt like something in my brain’s wiring had changed. That experience is what led me to explore the physiological causes of brain fog in acoustic neuroma—because for many of us, this is not just emotional; it’s neurological.

What the Research Shows
Research strongly supports that brain fog can be a direct result of the tumour itself, not just the emotional stress that comes after diagnosis. Several clinical studies have confirmed that people with untreated acoustic neuroma show real, measurable impairments in cognitive function.
A 2023 study of 75 untreated acoustic neuroma patients compared to healthy controls found that patients performed significantly worse in areas like memory, attention, processing speed, executive function, and visuospatial ability—all classic signs of brain fog. Importantly, these deficits appeared before any medical intervention, meaning they weren’t caused by surgery, radiation, or even the emotional weight of having a diagnosis.
Another earlier study found that 69% of patients with untreated tumours had clear signs of cognitive dysfunction, especially in alertness and visual-motor processing speed. Even advanced brain imaging like functional MRI shows changes in how the brain works in AN patients—reinforcing the idea that these symptoms stem from actual structural and functional brain changes, not just mood or mindset.
How Acoustic Neuroma Physically Disrupts the Brain
I am not a neurosurgeon or a brain scientist—but like many patients, I needed to understand what was happening to me. So I started digging, reading studies, watching expert webinars, and piecing things together. What I found helped me make sense of my experience—and I hope it does the same for you. While the science is still evolving, there are some explanations for why brain fog happens in acoustic neuroma.
So how exactly does a benign tumour like acoustic neuroma cause such profound cognitive changes—even before treatment begins? The answer lies in the physical and neurological effects the tumour has on the brain.
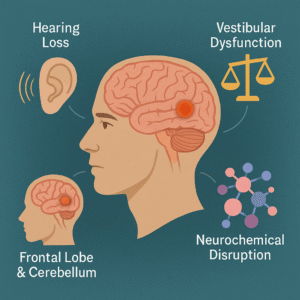
1. Hearing Loss Creates Cognitive Strain
Most acoustic neuromas affect one side of the auditory nerve, leading to unilateral sensorineural hearing loss. While that might sound like a simple ear problem, it forces the brain to work extra hard to decode speech and localize sound. This reallocates cognitive resources—especially from areas responsible for memory and focus. Studies show that even one-sided hearing loss can cause grey matter reduction in the frontal and auditory cortices, leading directly to cognitive fatigue and slower thinking.
2. Vestibular Dysfunction and Spatial Disorientation
Dr. Megan Sherrod explains in her ANA webinar, disruption of the vestibular system in AN patients affects brain regions like the hippocampus and parietal cortex—areas essential for navigation and spatial awareness. This sensory conflict can lead to what she describes as a cycle of dizziness, imbalance, and anxiety, making the brain work harder to maintain equilibrium and focus.
3. Frontal Lobe and Cerebellar Involvement
Though acoustic neuromas are slow-growing, they can press against the cerebellum and brainstem, structures now known to play a role in executive function, attention, and emotional regulation. Even smaller tumours—without obvious mass effect—can disrupt these circuits through network-level changes seen on functional MRI. Although some patients may appear outwardly “normal” or even perform adequately on standard cognitive tests, they can still experience real disruptions in attention, processing speed, and spatial awareness due to the tumour’s effects on key brain systems.
4. Neurochemical Disruption
The tumour’s impact on brain circuits also influences levels of neurotransmitters like dopamine, serotonin, and norepinephrine. These are the same chemicals involved in mood and cognition—and their disruption may contribute to a blend of brain fog, emotional flattening, and executive dysfunction. This might explain why brain fog in AN doesn’t respond to typical anxiety or depression treatments—it has a mechanical origin, not just a psychological one.
When a Name Brings Clarity
For many people, receiving a diagnosis like acoustic neuroma is understandably overwhelming. But for me, the experience was surprisingly different.
Rather than spiralling deeper into worry, I actually felt relieved. For months—maybe even years—I had been struggling with a kind of cognitive cloud I couldn’t explain. My thoughts felt slow. Conversations were draining. I knew something was wrong, but I didn’t have the language or validation to describe it.
So when I finally heard the diagnosis, it was like turning on a light in a dark room. I wasn’t just “tired,” “burnt out,” or “too sensitive.” There was a real, physiological reason my brain wasn’t functioning the way it used to.
In contrast to patients who feel worse after getting their diagnosis, I began to feel mentally lighter. My condition had a name—and with that came understanding, support, and, most importantly, a path forward. That shift in perspective didn’t make the symptoms go away, but it gave them context, and that in itself was incredibly empowering.
All I wanted to say today is that Brain fog in acoustic neuroma is not just “in your mind.” It’s a product of direct neurological interference, altered brain chemistry, and the body’s efforts to adapt.
And by acknowledging the biological roots, we can reduce the stigma and better support those living with AN—not by dismissing their symptoms, but by equipping them with tools to recover, adapt, and thrive.
It’s reassuring to know that you felt better once you knew what was causing your symptoms. I too was in the same situation but for a totally different problem. My issue relates to Non epileptic attack disorder. It took Doctors 4 years to figure out what it was that was making me collapse several times a day, often injuring myself. The sad news is there is no magic pill that I can take to stop them from occurring so I have to live with them & cope the best way I can.
As for brain fog & AN I see it in my wife. Where she was calm & controlled she is over emotional, she worries a lot more; perhaps more about our family then herself but she certainly worries a lot more.
The initial diagnosis came as a complete shock to her because she thought she was going to have a hearing aid fitted, the Consultant has since apologised for the way in which they handled the notification but none the less it has had a profound impact on her. So much so that I think she finds it hard to trust her consultant but I am working on that to reassure her that he is only working towards her best interests
Thanks for reading. I can understand
Thanks for sharing!
You have not only explained, but put the experience into words, Thank you!
Thank Chris
Hi can you send me this post please I have nf2
It’s public Heidi. You can share re share it
Your article definitely reached me. I too felt a sense of relief, I had suspected I had an AN for a few months and finally had an MRI which confirmed my thinking and it’s a 3 cm tumour. I’d suspected this or Mieniers disease. My GP had never heard of a AN before. For months I’d been back and forth feeling unwell and several diagnosises before confirmation of my tumour were ear infection, then stress and then high bloodpressure. Finally having an answer just made me feel like finally I’m not going mad, and this is what’s wrong with me. I’m apprehensive about surgery but know it’s the best outcome for my age as only 44. Thanks for sharing this.
Thanks Kitty. I am glad it resonated with you. All the best for surgery
ډېر ژور او د پوهې او ذاتي تجربې نه ډک ليک دى. د دې زمونږ سره شریکولو دپاره مننه، په خاص توګه د هغې خلقو د پاره چې هم د داسې تجربې نه تېر ووځي. د خپل ذهني او جسماني کيفياتو پوهنه او ادراک د هغې احساساتو او د ناروغۍ سره دمخامخ کېدو اولنۍ پوړۍ ده.
خداى دې صحت او نور توان، طاقت درکړي، دَ رحمان علي لالاجي خبره، خداى دې کال په کال ژوندى لره چې ډېرې اخترې او خوشالۍاووېنې، دخپلو بچو سره سېلونه وکړې
Grateful for your prayers and kind words
Better things come to those who wait but best things come to those who strive and fight…you’re such a great fighter. May Allah grant you healthy wealthy life ameen
قدرت دی روغ صحت سره د ډيرو خوشالي درکړي امين
It is good to see that you can write now so coherently. The post is informative and knowledgeable. Definitely got to learn a lot new things. I look forward to reading your thoughts on AN, neurology and on your personal experiences as well. Khushala osey.
Thanks Ashna,
My prayers always for you
Whilst this is extremely interesting I also find it very depressing. I also had a AN removed and suffered symptom post op . However I learnt how to help myself through excersise, a healthy life style and expert advice . Maybe I’ve been lucky
It’s good for AN patients to know what they are feeling is real but how about some words of encouragement on what may help them to feel better vs just confirming all the bad stuff . How can people suffering be given help ?
Great explanation pal!
Pingback: Clearing the Haze: How to Cope with Mental Fog in Acoustic Neuroma – Dr Amir Khesro
Pingback: Understanding Fatigue in Acoustic Neuroma: What It Is, Why It Happens, and How to Manage It – Dr Amir Khesro